News
News > Extract
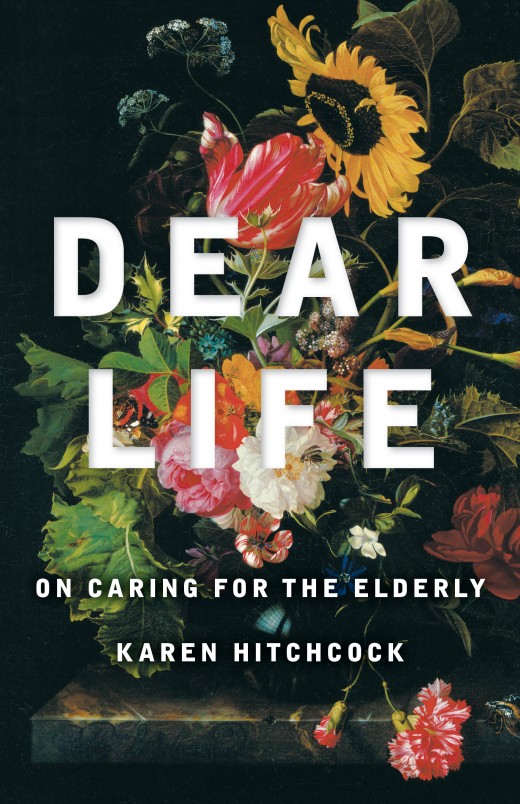
Read an extract Dear Life: On Caring for the Elderly by Karen Hitchcock
There are many ways to get sick, many ways to crumble and crash. I work as a physician in a big inner-city hospital overflowing with the sick. The orthopaedic ward is full of people who got up for a glass of water and snapped their hip. The psychiatry ward’s full of near suicides and phantom voices drilling holes in people’s heads. The cardiac cath lab’s overflowing with heart attacks. The burns unit usually has one or two people who tipped a bucket of petrol over their head and struck a match. We house the frail and the elderly, the drunken and the overdosed. Hearts and lungs are plucked from the brain-dead and sewn into the diseased; people crowd the emergency department, suffering because their organs are slowly failing the body that shelters them. What made them sick? What is health? What is it that we do to people in a hospital?
We elders have learned a thing or two, including invisibility … When I mention the phenomenon to anyone around my age, I get back nods and smiles. Yes, we’re invisible. Honored, respected, even loved, but not quite worth listening to anymore. You’ve had your turn, Pops; now it’s ours. — Roger Angell, 93
There are many ways to get sick, many ways to crumble and crash. I work as a physician in a big inner-city hospital overflowing with the sick. The orthopaedic ward is full of people who got up for a glass of water and snapped their hip. The psychiatry ward’s full of near suicides and phantom voices drilling holes in people’s heads. The cardiac cath lab’s overflowing with heart attacks. The burns unit usually has one or two people who tipped a bucket of petrol over their head and struck a match. We house the frail and the elderly, the drunken and the overdosed. Hearts and lungs are plucked from the brain-dead and sewn into the diseased; people crowd the emergency department, suffering because their organs are slowly failing the body that shelters them. What made them sick? What is health? What is it that we do to people in a hospital?
Fundamentally, it would seem, a doctor’s job is to treat and protect diseased and threatened organs – those beautiful and intricate and faithful structures that pump and squeeze and metabolise away, mostly quietly, keeping us alive. Just treat them, doc, and go home. How difficult can it be? But when doctors sit in consulting rooms or walk the wards, we don’t confront kidneys and hearts. We encounter complex, imperfect, suffering people with specific histories, cultures and understandings of sickness and health. And we do this, for the most part, within institutions with vast management structures whose role is to maintain economic viability and safety. We do it within government-dictated fiscal constraints. The business of health care is something much more than a delivery of goods and services.
The medical system is constructed from tacked-together fragments – GPs, specialists, the hospitals, mental health services, community services – all of which have little contact with each other. We treat social and medical needs separately, although they are intricately entwined. Hospitals themselves are designed around a body fragmented into discrete organs. Often, our institutions serve clinicians, bureaucrats and cutting-edge science better than those they are supposed to be serving.
Most of my patients are old. This new longevity of ours is a triumph. I have had patients who are over 100 years of age and still live at home. I see them and feel wonder and hope. But the health system – and society – is struggling to adapt to our ageing population. At times it seems we are struggling against it.
In 1976 Robert Neil Butler, an American geriatrician, won a Pulitzer Prize for his book Why Survive? Being old in America, in which he coined the term “ageism.” In Why Survive? Butler outlines many ways the elderly are neglected in society and shut out of the medical system. Five years earlier, in France, Simone de Beauvoir published The Coming of Age, in which she too describes a society where the elderly are forgotten, discarded or despised. Both books are rigorously researched and statistic-heavy. The points the writers make are as relevant today as they were forty years ago.
It is difficult to improve the care we offer our elders – in and out of hospital – when, as Linda Marsa writes, we are fearful of “the swelling ranks of ‘greedy geezers’, the oncoming grey tsunami of the sick and frail elderly who will be an emotional and financial burden on their families and friends, and whose infirmities could bankrupt the healthcare system.” We hear a continual cry that our healthcare system is “unsustainable”; that the healthcare needs of ageing baby-boomers may bankrupt the country. Age discrimination in medicine is widespread, although often hidden behind many benevolent aims: the promotion of patient autonomy, the wise allocation of health resources, the avoidance of what is futile, the primacy of quality of life. Our response to age-related memory loss and dementia is to institutionalise, isolate, sedate. Supporting independence and wellbeing in old age remains a low priority.
One of the most-read articles in the Atlantic in 2014 was “Why I Hope to Die at 75” by a professor of bioethics, Ezekiel Emanuel. In it, he jauntily promotes the idea that it is a horror to grow old; that growing old necessarily involves the accumulation of disability, the transformation of a human subject into a wreck and a burden on family and society. Emanuel’s answer to his dire evaluation of elderly life is to die early. There’s a picture of him, a man in his late fifties, radiating vitality, sitting with his feet up on his desk, long legs crossed, drinking from a cup that says “The Boss.” Another picture shows him with his arms slung around two of his nephews at a base camp of Mount Kilimanjaro, which the three climbed. Accompanying the article is a bright yellow graph that depicts the decline in one’s productivity with increasing age. Emanuel knows his place – as the boss, at the top of the mountain, at the peak of a very particular kind of productivity – and he would rather die than give it up.
There are many ways to show that we devalue our elderly, are repulsed by them, terrified of becoming them. They have been and remain the last priority in our medical system and the ones we target first with our austerity measures. This book does not offer simple solutions to the structural inadequacies it diagnoses. The solutions are not simple. My chief aim is to strike a note of caution and to make explicit something that often remains unsaid and yet can be heard quite clearly: that the elderly are burdensome, bankrupting, non-productive. That old age is not worth living.
Share this post
About the author
Dr Karen Hitchcock is a general physician whose clinical work has focused on pain, fatigue, medically unexplained symptoms and obesity. She holds a PhD in English and writes regular essays for The Monthly. She is the author of the Quarterly Essay Dear Life and the story collection Little White Slips, which won the Steele Rudd award in the 2010 Queensland Premier’s Literary Awards. Hitchcock was one of the first authorised prescribers of medicinal cannabis in Australia.
More about Karen Hitchcock